Psychological Trauma and Posttraumatic Stress Disorder
Stress and trauma are common human experiences. While stress is a normal response to new and challenging situations, trauma involves an overwhelming response to life-threatening situations, injury, or sexual assault. Stress is not always harmful, but trauma almost always is.
The most common forms of trauma in Australia are:
The unexpected death of a loved one;
Witness to a person being severely injured or killed, or finding a dead body; and
Life-threatening motor vehicle accidents.
There are also occupational exposures, in particular military trauma and trauma in first-responders and corrections officers.
The outcome of trauma is widely variable. It depends on genetic factors, history of prior exposure to trauma, and physical injuries sustaind at the time of trauma. Posttraumatic Stress Disorder (PTSD) is not an inevitability of trauma. Other potential outcomes are Acute Stress disorder (ASD) and Posttraumatic Growth (PTG).
What is PTSD?
PTSD is a syndrome of stress reactions that can develop following trauma. These reactions are clustered within four categories: intrusive symptoms (nightmares and flashbacks), avoidance symptoms (flight response), negative changes in thoughts and mood, and heightened arousal (fight response - startle, hypervigilance, anger). These symptoms must be present for at least a month and must cause significant psychological, social, or functional impairment. ASD is similar to PTSD but the symptoms resolve within the first month.
There can also be symptoms of feeling as though you’re outside your body, or feeling as though you’re on autopilot, or the world is in a bubble or a simulation, or sometimes where patches of memory are lost. These dissociative symptoms are present in the more severe forms of PTSD, particularly where there is prolonged exposure in childhood.
Complex PTSD arises from prolonged exposure to trauma and involves difficulty controlling emotions and difficulties in relationships. This differs from Borderline Personality Disorder (BPD), which doesn’t have some of the core features of PTSD and involves other psychological defence mechanisms.
It is also important to mention Moral Injury in discussion about PTSD as it shares some of the same features of PTSD and complex PTSD, and often occurs alongside PTSD. This is a relatively new and complex concept that describes the effects of violating a person’s moral code rather than from exposure to a traumatic event. The hallmarks of Moral Injury are shame, grief, guilt, self-condemnation, self-sabotage, hopelessness, and loss of meaning.
Why does PTSD emerge?
Professor Richard Bryant of the University of New South Wales recently reviewed the scientific literature on PTSD. He identifies three models of why PTSD emerges:
Neurobiological models;
Genetic vulnerability; and
Cognitive-behavioural models.
The truth probably lies within a combination of all three, with variances from person to person. However the two that open up therapeutic targets are the neurobiological models and cognitive-behavioural models.
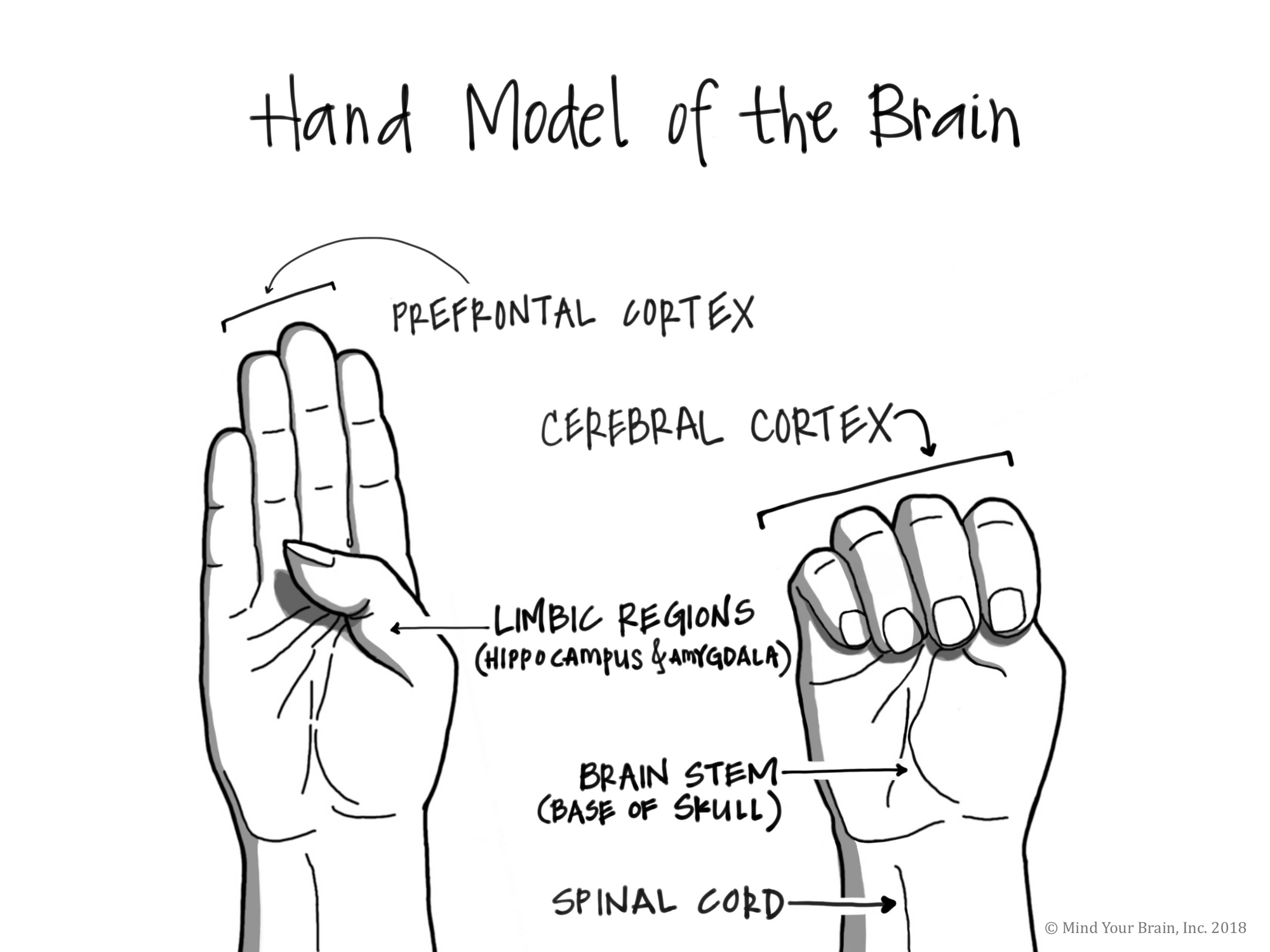
The neurobiological model is based on fear conditioning. In this model, stress hormones released at the time of the traumatic event lead to a strong association between trauma cues and fear responses. This involves the emotional and memory circuits of the limbic system (the hippocampus (long term memory) and the amygdala (which is always on the look out for danger based on past experience)) and the prefrontal cortex (where conscious awareness is located).
I like using Dr Dan Siegel’s hand model of the brain to talk about this with patients. It’s a great broad brush sketch of the complex neurobiology of stress.
In this model, the amygdala has a direct link to the fight-flight or freeze-dissociate responses, which is much faster than conscious awareness inhabiting the prefrontal cortex. This explains why people with PTSD will often be unable to explain what triggered them.
And you can see how the symptom clusters of PTSD link directly to this model. The limbic system triggers the arousal (fight), avoidance (flight), intrusion (fragments of traumatic memories), and dissociation symptoms due to increased sensitivity to external stimuli that are reminiscent of traumatic exposures. Meanwhile the prefrontal cortex struggles to regulate the limbic system, which in turn impacts cognition and mood.
A rational approach to prescribing medication PTSD is to use this neurobiological basis to guide medication choice. The goal is to essentially bring the prefrontal cortex back “online” so that the person can benefit from psychotherapy. Psychotherapy is at the core of treatment, but medication enhances its effect by helping to strengthen disrupted brain circuits.
This is where the cognitive-behavioural model comes in. These models focus on the fact that traumatic memories are encoded in sensory fragments with disorganised sequences. This in turn limits the way that these memories can be integrated with more “adaptive memories” within the overall autobiographical memory.
A lack of integration results in a bias towards threatening stimuli. And so a vicious cycle ensues through the neurobiological circuitry, whic leads to the psychological, social, and functional impairment seen in PTSD.
Trauma-focused psychotherapies essentially aim to restore that integration so that the vicious cycle can be broken down. But you can imagine how difficult this can be - in therapy, you’re fighting against evolutionary processes.
Towards posttraumatic growth
As I noted before, PTSD is not the only outcome. Traumatic experiences are potent experiences that can disurpt the way that a person sees themselves and the world. The response to such a tectonic disruption can lead to growth in some people. Posttraumatic growth is a more recent concept that has emerged from Positive Psychology that is important to touch on, though it’s not entirely clear how this can be incorporated into clinical practice.
Posttraumatic growth is different from resilience. Whilst resilience is the capacity to “bounce back” from adversity, a resilient individual may not necessarily experience posttraumatic growth. Growth after trauma occurs through the struggle that can ensue following a traumatic incident. Through that struggle, the person will confront deep existential challenges that have been thrown up as their worldview and sense of self has been disrupted.
Indeed, posttraumatic growth may occur through recovery from PTSD. To me, the role of the clinician in that journey is to go with compassion alongside the person with PTSD and help to equip them with what they need to confront their monsters.
But care must be taken as our own monsters can be stirred up along the way.